Sweden and Covid: unraveling the mystery
Sweden suggests that half-hearted Covid restrictions were not very effective
My global deep dive on Covid statistics left out one of the most hotly-debated countries: Sweden 🇸🇪
That’s because it deserves its own investigation. Sweden is an important case study, as it steadfastly avoided lockdowns, even while its neighbors had more typical restrictions.
Yet, Sweden is a bit of a mystery, as it’s cited both by people who support restrictions, and by those who oppose them. Here’s why:
1. Sweden had more deaths than its nordic neighbors
First, let’s Zoom in on my Covid19Mapped.com map of excess mortality during Covid:
We can see that, as of Jan 1, 2022, Sweden was doing worse in excess mortality1 than all its nordic neighbors. Here are the numbers for all five Nordic Union countries:
Excess deaths during Covid
Sweden: 1075 deaths per million
Denmark: 635
Finland: 516
Iceland: -19 (fewer people died in the Covid era than in the pre-Covid era)
Norway: -30
This comparison looks bad for the Swedish model. But, what about:
2. Sweden had fewer deaths than most of Europe
Out of 22 EU countries (putting other nordic and tiny countries aside,) Sweden did better than all but Ireland.
Between these two facts, what can we say?
First, one has to admit that the situation is complex. Sweden is not a simple “restrictions worked!” or “restrictions didn’t work!” story.
Instead, the data are telling us: partial restrictions are not the primary factor in determining a country’s success with Covid.
As we saw in the last investigation, the same cannot be said for all-out restrictions; the few countries that combined near-total travel bans with sporadic lockdowns unambiguously kept Covid at bay and dramatically reduced Covid deaths. Strict rules saved lives, but that came at a cost to freedom.
Europe, and most of the world, took a more half-hearted approach. Often, they had some policies that were very strict, while allowing other Covid vectors to remain (such as allowing international travel and public transport.) The various mixes of policies failed to prevent exponential spread of the virus.
But did they at least save some lives, compared to Sweden’s hands-off approach? The above maps suggest they were not the biggest factor, but they may still have helped.
Let’s dig further, to find out:
3. Nordic culture lends itself to fewer cases, so comparisons to non-nordic Europe may not be valid
In deciding which of the above maps to put more weight on, we should realize that the nordic countries have a distinct culture.
For example, nordic countries are very individualist when it comes to family relations, as can be seen in this map:
These data show that in Southern and Eastern Europe, people are much more likely to live in inter-generational families, something that spreads Covid from young people to older ones. The nordics are an extreme outlier, with a 10 times smaller share of young adults living with parents than in some southern countries.
Less quantifiably, nordic people are known to be “colder” — to associate more with very close friends, and less with strangers and acquaintances — and to want more personal space.
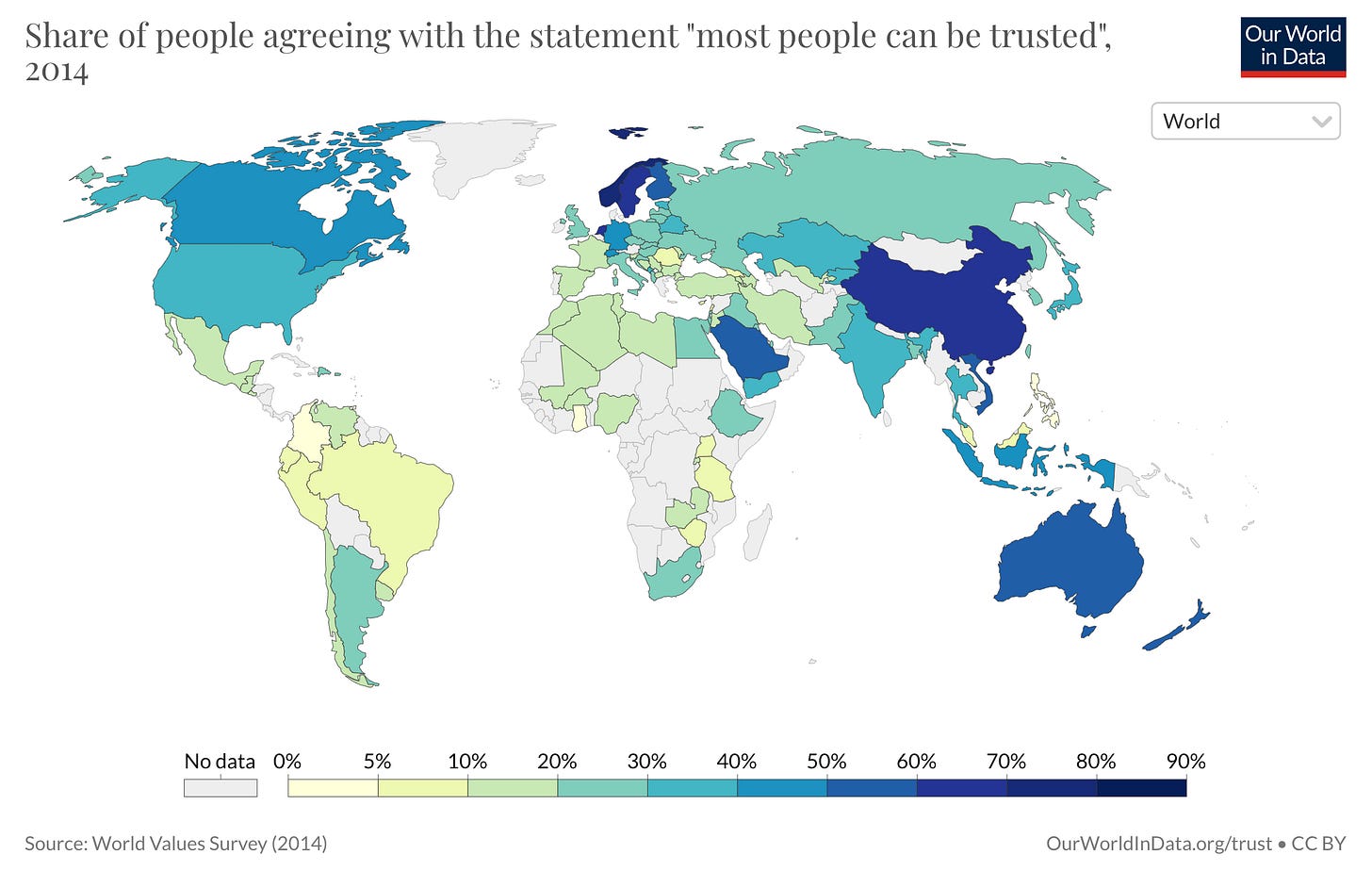
Also, nordic people have uniquely high trust in others (which extends to trusting their governments, including when it comes to following advice about viruses):
Also, nordic countries tend to be wealthier:
So, while Sweden did better on Covid deaths than almost all of Europe, perhaps that should be expected — as it also has higher incomes than almost all of Europe.
There are many other regional factors that we undoubtedly missing. I learned just recently that bacterial antibiotic resistance varies greatly by region — which is important, because death is often caused by secondary bacterial infections.
Here’s a map of antibiotic resistance for one kind of bacteria, which is a somewhat common Covid secondary infection, representing about 15% of secondary infections:
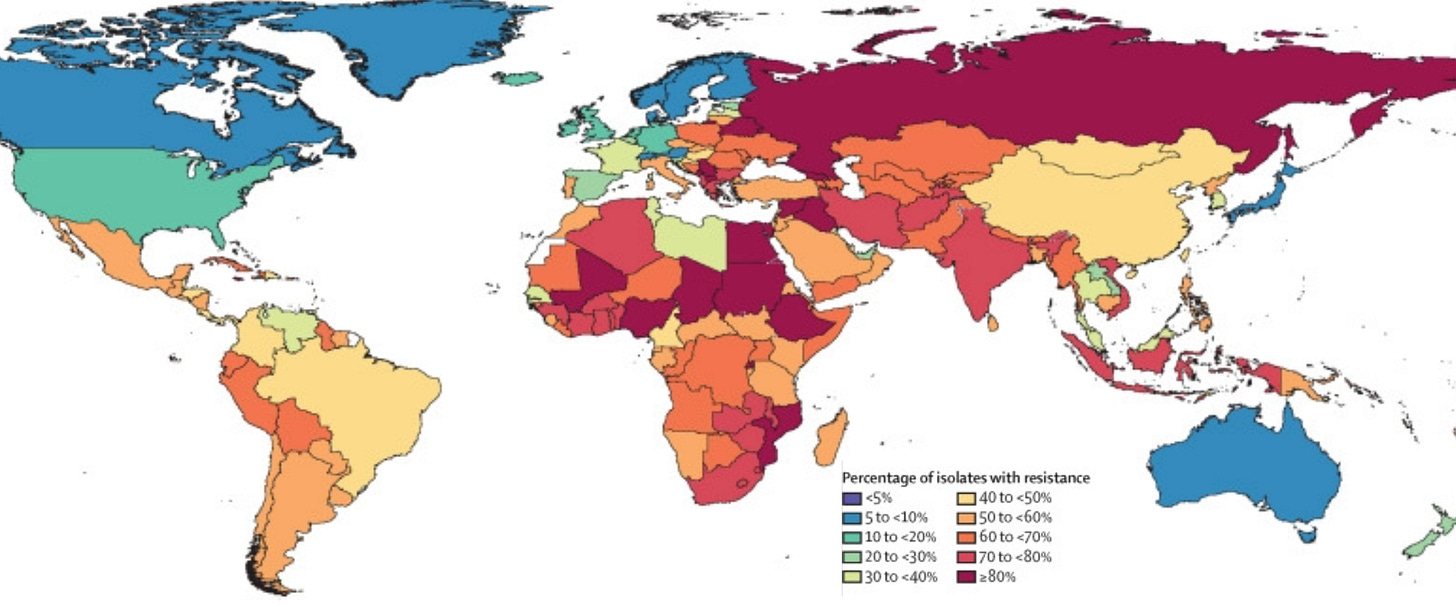
We see that the nordic countries are an outlier in terms of having bacteria that are still treatable with antibiotics.2
The big differences shown above lend support to the notion that it’s fairest to compare Sweden to its nordic neighbors.
There are substantial differences within the nordic countries, as well (in particular, Sweden has more immigrants, and a larger capital city) but they are almost certainly smaller than the differences between Sweden and non-nordic countries.
Below, we’ll Zoom in on the nordic countries.
4. Nordic data in detail
I apply the same analysis that I used in my last post. First, cases:
We can see that Sweden was different from the other nordics in that it did not keep cases low early on, which makes sense, as its policy did not try hard to keep them low. Instead, Sweden’s equivalent of Dr. Fauci talked up reaching natural herd immunity at the start, and how Sweden trusted its citizens to make their own decisions.
The graph also shows that all the the nordic countries eventually converged to have similar rates of cumulative cases, except for Denmark – but that appears to be mostly an artifact of the country having much more widespread testing.3
Now let’s look at official Covid deaths, as labelled by governments:
Here we see that fatality rates were much higher in the original and Delta-waves, before the virus weakened and vaccines became available.
Sweden had a lot more deaths early on than did the nordic countries with more restrictions.
But the excess mortality data complicate the picture. The graph below shows all extra deaths — not just the officially-labelled Covid deaths:
This data hint at Finland undercounting its Covid deaths during the Omicron wave.
That was also reflected in the global “fudge factor” map in the last post:
As a result, Sweden has actually had no more excess deaths than Finland had, despite Finland’s stricter rules.
How much stricter were they? For example, on March 16, 2020, Finland closed all universities and schools (except for the children of front-line workers) through June 1, 2020. Finland also banned all gatherings of 10 or more people.
Sweden only banned gatherings of more than 50 people. And it continued in-person schooling at the elementary and middle school levels. Sweden was the only country in western Europe to have always avoided closing all its primary schools.
Perhaps as a result, a 2022 study found “No learning loss in Sweden during the pandemic.” While I don’t see a comparable study on Finland, national test data in the US shows plummeting test scores following school closures.
Just generally, Finland was somewhat stricter than Sweden. In the Omicron wave, it too avoided closing all schools, but it forced restaurants to close by 6pm. In Sweden at the same time, restaurants were forced to close by 11pm. Those five hours surely make a big difference to a restaurant business.
Yet the excess mortality data suggest that Finland’s extra measures were almost wholly ineffective. This is in line with some specific study findings as well, like one titled, “Closing lower secondary schools had no impact on COVID-19 incidence in 13–15-year-olds in Finland.”
Of course, it remains possible that Finland would have done worse than Sweden if it hadn’t had restrictions, and that it needed them to achieve parity. But as far as we can tell, the extra half-hearted restrictions in Finland had no positive effect. (Note: Finland is a bit less rich than Sweden, but it also has far fewer immigrants, and smaller cities; it’s not at all obvious which country one would naturally expect to do better.)
Norway managed to keep cases low thanks to a strict 2-year-long travel ban, avoiding about 40% of Sweden’s extra deaths.
But the graph shows that Norway, too, might be starting to catch up to Sweden in excess mortality. I’ll be interested to see what the data looks like at the end of the year.
Partly, the catch-up in excess mortality (which is not seen in official Covid death count) may be an illustration of the reality that if you prevent a 90-year-old from dying of Covid in March 2020 — well, many such people are going to die by September 2022, even if kept safe from Covid. So part of the catch-up is because some of the “lives saved” unfortunately couldn’t be saved for very long.
This is one additional way in which the second chart (the official Covid death count) can be misleading even when true: It counts all deaths equally, regardless of long someone has to live, regardless of Covid.
Every death is tragic, but, if a person is going to die anyway the following year, I think people understand that it’s less tragic than someone cut down in their prime. The excess mortality chart is illustrating some that reality already (and as time goes on, it’ll do so increasingly. After years, we should expect the lines to get close, even if prevention was really effective.)
That discussion leads us to:
5. Cost/Benefit analysis
In the previous deep dive, we saw how Australia and New Zealand — by going all-out to keep Covid cases near zero — saved themselves roughly 2 weeks of life for every person in their country, on average.
That didn’t seem worth it to me, but some would legitimately disagree.
In that post, I compared total-control Australia with the US’s mix of half-measures.
What if we compare between relatively-germ-resistant nordic countries? Comparing effective-travel-ban Norway with no-lockdown Sweden?
Based on the cost-benefit calculations from the last post, it appears that Norway saved about a total of about 2,200 lives compared to Sweden’s approach, which is about 1.8 days of life per Norwegian resident.
To the extent that the people who died were unhealthy for their age group, it may be less than 1.8 days. But, to the extent that vaccines and Omicron would have made cases milder for those who survived regardless, it’s reasonable to think that Norway also spared its residents some days of misery from Covid symptoms.
Comparing Denmark and Sweden, it appears that restrictions saved about 3,900 lives, or 2.9 days of life per Danish resident, if their alternative were being like Sweden.
In Finland, of course, the effect seems to have been zero.
So our estimate is that nordic restrictions beyond what Sweden implemented saved roughly around 0 - 2.9 days of life per resident.
It should be noted that Nordic countries are safer in general. For example, while in the United States, driving deaths over two years represent about 3.3 days of life lost for every person, Sweden’s population-adjusted driving death rate is a massive 75% lower.
So, proportional to other common risks, the small Covid gains from restrictions within the nordic countries do look a bit less small.
It’s also worth keeping in mind that the differences between Sweden and its nordic neighbors4, such as Sweden having more migrants, a bigger capitol city, and a milder previous flu season, may also explain Sweden's slightly higher rate. This study finds that Sweden's mild flu season would account for about 19% of the deaths during the first wave.
It’s possible that all the factors add up 100% of the difference from restrictions, though I doubt it. Canada’s experience may be worth looking at, as it has a comparable number of immigrants, cities bigger than Stockholm, a similar climate, and strict lockdowns; it did better than Sweden on Covid deaths.
We can’t say for sure that the restrictions had any positive impact. But our first-line analysis here gives weak evidence that they helped a bit.
Added Sept 14, 2022: Scott Alexander has another interesting way of illustrating the cost-benefit tradeoff. He calculated:
[if Sweden had imposed typical European lockdowns, then] every 52 months of stricter lockdown … would have saved one month of healthy life. You will have to decide whether you think this is worth it, but it seems pretty harsh to me.
… [even if] strict lockdown has 100% efficacy and prevents every single COVID case… it’s 21 months of stricter lockdown to save one month of healthy life. Again, seems pretty harsh.
Conclusions
Sweden is not a clear-cut example for either the pro-restriction or anti-restriction side, but it does weigh against particularly painful restrictions, by showing how hard it is to definitively pin down a positive impact from them.
Sweden does show that restrictions were not the primary factor in determining deaths rates.
A first-line analysis suggests that restrictions had between zero impact, and a small positive impact, which would be a bit less small when viewed in proportion to the already-safe nordic environments.
The extra restrictions imposed by Sweden’s neighbors probably fail a cost-benefit analysis, in that most people would have preferred to give up the days than deal with the extra restrictions. But people should come to their own conclusions on that.
I hope you found this post interesting. Please consider hitting like, or sharing it:
Also consider subscribing below, to get more posts like this one:
If one looks at official government Covid death counts, the pattern is similar.
It’s quite surprising to me that bacteria vary so much from country to country, but that’s what the study in the Lancet found. I guess many bacteria are much less mobile than airborne viruses like Covid. Note: See image D in that study for the most common Covid secondary infection. There, the pattern is less stark vs non-nordic Europe, but again the nordic countries do very well.
Denmark was more serious about testing. Here are the testing positivity rates during the Omicron wave (Dec 1, 2021 - March 1, 2022)
Norway: 44% positive
Sweden: 28% positive
Finland: 25% positive
Denmark: 16% positive
What this shows is that Denmark administered 2.75 as many tests per detected case as Norway did, and 1.75 times as many as Sweden did.
So Denmark’s massive difference with other nordics on the cases chart is mostly just due to testing more. (The same cannot be said about its difference with the US, but that’s not so relevant here.)
Some argue that Sweden isn’t very comparable to nordic countries, either. Klein et al point out 16 different factors. Here are their strongest points, many of which are no doubt hurt Sweden in Covid deaths:
(1) the “dry-tinder” situation in Sweden (we suggest that this factor alone accounts for 25 to 50% of Sweden's COVID death toll);
(2) Stockholm’s larger population;
(3) Sweden’s higher immigrant population;
In an interview for UnHerd, Sweden’s chief epidemiologist Anders Tegnell said: “Sweden is quite different from our neighbors,” and: “The population looks a lot more like the population in Netherlands, Belgium or the UK – with a high level of migrants and quite big areas of densely populated cities around Stockholm.”
(4) in Sweden immigrants probably more often work in the elderly care system;
(5) Sweden has a greater proportion of people in elderly care; …
(7) Stockholm’s system of elderly care collects especially vulnerable people in nursing homes. …
(10) Sweden may have been slower to separate COVID patients in nursing homes;
These appear to be valid points, and make Sweden’s higher rates possibly not due to lack of restrictions at all, but rather due to these differences.










> Out of 22 non-Nordic EU countries, Sweden did better than all but two of them (Ireland and Switzerland.)
Switzerland is not a member of the EU.
Thank you for this. At the time, Sweden's more relaxed approach presented a fascinating test case and it's good to see a rigorous analysis of the possible effects of this approach.
This paragraph raises a technical question in my mind:
"Partly, the catch-up in excess mortality (which is not seen in official Covid death count) may be an illustration of the reality that if you prevent a 90-year-old from dying of Covid in March 2020 — well, many such people are going to die by September 2022, even if kept safe from Covid. So part of the catch-up is because some of the “lives saved” unfortunately couldn’t be saved for very long."
In the operational definition of "excess mortality" that you've used, is the figure cumulative for the entire period, or a month-by-month calculation based on expected death rates for those alive in each period?
In other words, in expressing the excess death rate for the period of January 2020 through July 2022 for the age group 85-90 (for example), does that reflect the aggregate deaths versus the expected deaths (based on the earlier comparison period) for the time period viewed as a unitary whole or does it represent the sum of each month's excess death rate based on the number of people alive at the beginning of that month?
To me, it seems that the latter measure (if feasible) would tend to avoid the "catch-up" effect that you point out. In the cumulative model, the mere fact that the countries that avoided early deaths would mean that there are just numerically more old people left alive who can die. But if that larger group of old people are dying in July 2022 at *rates* no higher than they died in the comparable earlier period, there should be no "catch-up" effect.
I'm no statistician, so I readily concede that what I'm saying here might not make much sense at all.