DEEP DIVE: Does Covid Cause Significant Brain Harm?
"Covid and brain tissue loss confirmed,” I read on the excellent blog Marginal Revolution.
The link goes to this fascinating UK study, which scanned tens of thousands of brains before Covid, and then scanned many of the same ones again, after Covid hit.
Here’s what I learned from digging into that study and others:
— Brain scans reveal effects on the brain that are relatively minor compared to typical non-Covid-related changes in brains over a 3-year period.
— Brain scans reveal an age-specific impact on the brain, with people under 60 having no significant difference and people over 60 having a more noticeable (but still not huge) negative impact.
— “Long Covid” is real, especially regarding sense of smell, but it is also rare.
— Most media headlines on these issues have been irresponsible in overstating the level of brain harm a typical person should expect.
Now let’s go through the study details!
The study cited by Marginal Revolution examined changes over time in the brains, comparing people who did and didn’t get Covid.
Their intro describes: “…loss of grey matter in limbic cortical areas directly linked to the primary olfactory and gustatory system.”
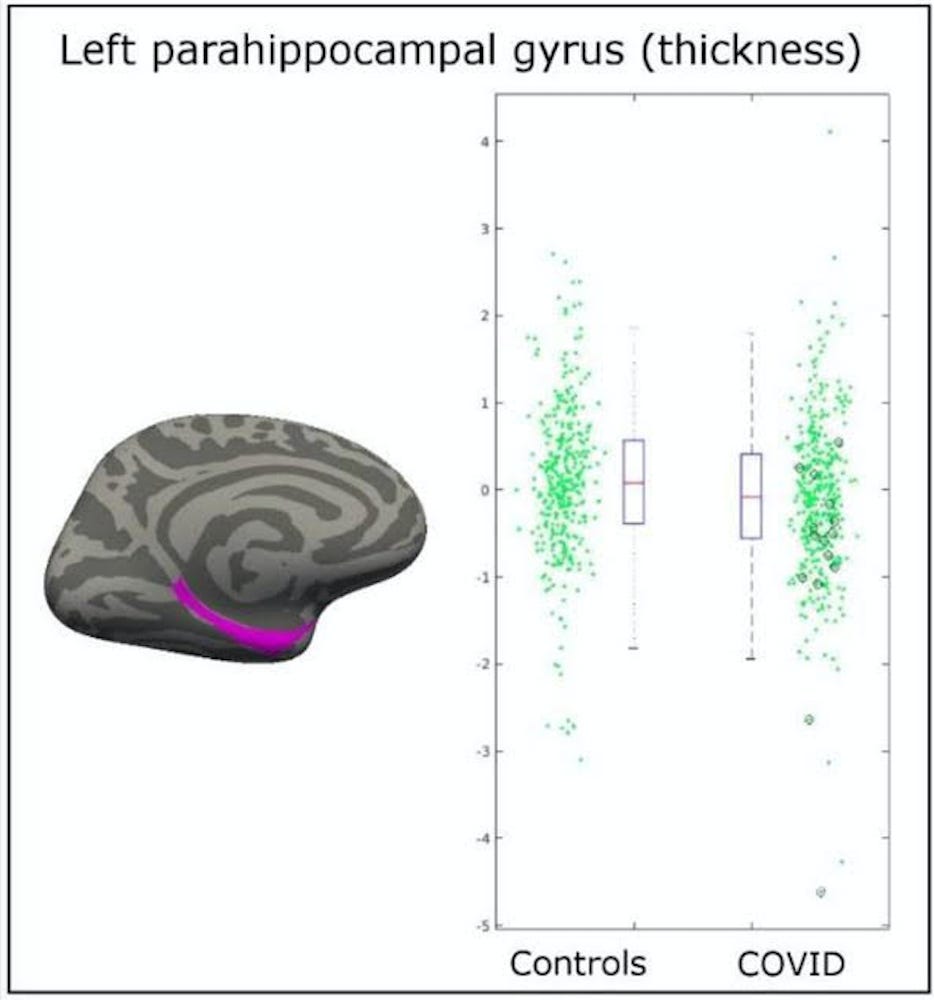
Now let’s look at the data. Here’s Figure 1 in the paper:
On the left, they have a scatterplot for “Controls” — people who did not get Covid. Each dot above 0 indicate a brain that gained matter relative to others, and below 0 indicates brain loss. All subjects were over age 45, and each green dot represents the change in each person’s brain over 3 years.
On the right, we have the same plot for people who did get Covid. Notice that the mid-point of the scatterplot is ever so slightly below that of the non-Covid group. This is the negative effect of Covid.
But importantly, and ignored — the small difference in the averages of the two plots is nearly invisible compared to the typical change in brain density that an adult’s brain goes through in a 3-year period.
It’s possible that Covid does something specific to the brain that the researchers just can’t measure — but with the brain scan technology we have, this study shows Covid is a drop in a bucket of other effects.
We know that all sorts of things also have an impact on the brain, from other illnesses like the flu, to alcohol, to stress and sleep deprivation, to poor eating and exercise, to watching too much TV and failing to stimulate one’s brain, to endless other conditions.
Up against those things, Covid only represents a couple percent of the typical variation in brain loss/development over 3 years.
If one is worried about maintaining brain function, the attention one devotes to avoiding Covid shouldn’t outweigh the attention one gives to the other factors above.
An additional note: the black-circled dots in the chart represent people hospitalized for Covid. These are more clearly on the lower-end of 3-year brain development, but also not off the chart.
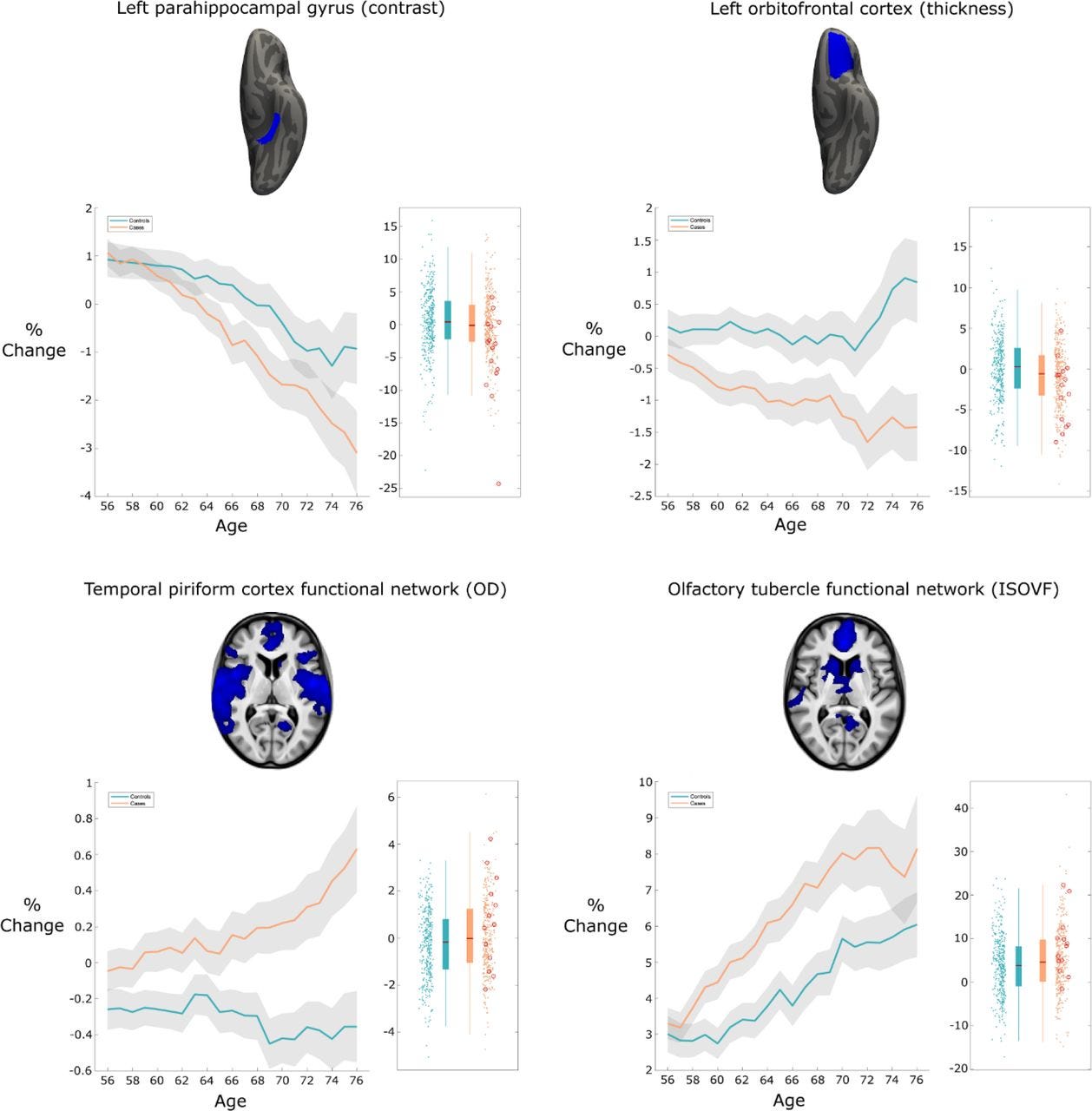
The researchers looked at multiple regions of the brain, finding similarly in all regions for which they display data:
That seems fairly clear-cut.
There’s also more to learn from their data. A month later the same researchers released an updated paper with an age breakdown.
The following chart is the same as the upper-right chart in the above image — but now with an age breakdown, on the bottom axis. It shows that at age 56, people who did have Covid (orange) and didn’t (blue) are similar, but the older people in the study who had Covid saw a more noticeable decline.
Side note: “% change” does not straightforwardly mean % change in brain matter — it’s been “normalized”, and means the change relative to a typical brain change during the study duration. The study also notes that these most-affected brain regions are those that most relate to sense of smell.
The study’s age-related finding holds up across the most-impacted brain regions.1 The researchers also look at total brain volume, and these data show the same trend.2
Beyond brain scans, the researchers also did cognitive tests on people, both before and after Covid. Two of the nine tests showed a significant difference — but again, only for people over age 60.
These charts show the difference across different age groups for those 2 tests; with age of subjects on the bottom; orange lines show the change in the time it took for people who had Covid to complete tests, and blue lines show the controls who didn’t get Covid.
These two cognitive tests both involve connecting numbered/lettered circles on a page quickly and in correct order.
Older people may be at higher risk of cognitive loss from Covid — though overall, per the scatterplots, the effect is still quite small.
But haven’t we seen more dramatic claims elsewhere, based on other studies?
There are lots of media headlines like:
PBS: Study Finds Cognitive Deficits in People Who Had COVID
Telegraph: Covid-19 can impact intelligence, says study
These articles were based on a different study in the Lancet titled “Cognitive deficits in people who have recovered from COVID-19.”
Some of the paper’s conclusions sound scary. The one time the paper gives a concrete comparison to IQ points is here:
“The scale of the observed deficit was not insubstantial; the 0.47 SD global composite score reduction for the hospitalized with ventilator sub-group was greater than the average 10-year decline in global performance… in a classic intelligence test, 0.47 SDs equates to a 7-point difference in IQ.”
In other words, if you have Covid and it’s so bad that you have to go on a ventilator, the study suggests that you may suffer a large (7 point) drop in IQ. That’s not so surprising, considering that about half of people put on ventilators actually die.
But what about typical cases? The paper suggests that has an impact about 7 times less than a ventilation case, measured in standard deviations, suggesting roughly a 1-point loss in IQ.
Not great, but also hardly life-changing.
But we should be skeptical. Critically, the study isn't “longitudinal”. The first study was, meaning it compared changes in the same individuals at different periods in time (pre- and post- Covid.) That’s a good design. But this second study merely looked at a bunch of people at a single point in time in the post-Covid era and compared those who had Covid with the others.
The well-known problem with that method is that people who did/didn’t get Covid might differ in important ways, beside Covid itself.
So if lower-IQ people tend to be less worried about Covid, then even after controlling for education and income — that would exaggerate the negative effect they find for mild cases.
For the ventilator case, too, they are likely missing important confounding variables. Low-IQ may correlate with pre-existing conditions; the authors control for several things, but don’t control for e.g. obesity, a known major risk factor for severe Covid.
Those are just two out of a staggering number of possible missed variables that could exaggerate the effects.
Overall, I’d discount this study (except perhaps to consider it as an upper-bound for the harm of Covid.) The brain-scan one is better designed.
Long Covid? Beyond brain density / IQ
The above all ties into general concern about “Long Covid”, which indisputably happens to some people.
If one reads media headlines, one will certainly be scared:
TIME — Almost 25% of COVID-19 Patients Develop Long-Lasting Symptoms
The Hill — Study: 37 percent of COVID-19 patients report at least one long-term symptom
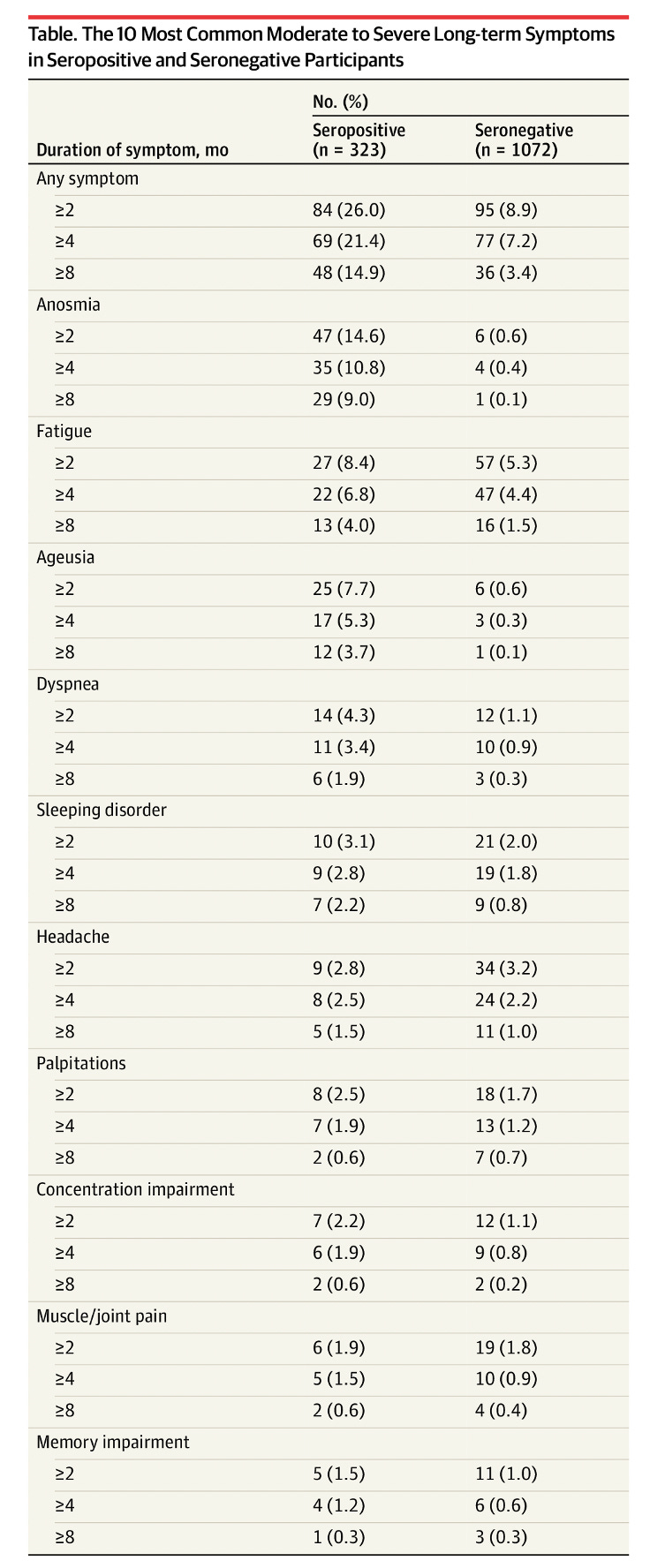
The best-done study on this is from Sweden, with about 2,000 medical workers. It shows that people who had Covid (positive for antibodies) had higher rates of long-term symptoms than did people who were negative.
After 8 months, 9% of the Swedish medical workers who had Covid still reported a loss, or change in, smell (medical jargon word: “anosmia”) compared to virtually nobody in the negative-for-antibodies group.
3.7% also reported lingering loss of taste (“Ageusia”) after 8 months:
However, other lingering symptoms are rare: 4% of people who had Covid reported fatigue after 8 months, compared to 1.5% of people who never had Covid.
The data suggest that in the general population, about 1.5% of people would be reporting fatigue anyway; we should subtract this from the Covid number to get the extra effect of Covid.
So, 4% minus 1.5% = ~2.5% chance of long-term fatigue due to Covid.
Other long-term effects caused by Covid are even rarer. Shortness of breath (“dyspnea”) is under 2% after 8 months. Everything else is near 1% or less.
UK data is also consistent with the Swedish findings.3 One side note is that they find all ages are at similar risk of reporting long Covid symptoms.
This all suggests that long-run effects are a risk, but quite small.
Long-term loss of smell is by far the biggest risk.
I had Covid in September 2020, and I totally lost sense of smell. I resigned myself to the possibility it might not come back, and was already planning out an alternative career in sewage plant maintenance.
But then it did fully come back, starting around 2 weeks, and came back gradually and linearly, until it was totally normal by 8 weeks.
I didn’t much mind not having a sense of smell — it was fine. But other people might value it a lot.
The other risks are quite rare.
Also, these numbers should be considered an upper-bound because of a possible “nocebo effect.”
The “nocebo effect” is like a “negative placebo effect”, and it happens when someone thinks they have a problem merely because their brain is expecting a problem. What the person feels is real, but it’s a psychologically-caused problem, not a physically-caused one.
Placebo effects are a significant issue — so much so, that it’s a requirement in clinical studies to give some people a placebo, to make sure that the drug isn’t “working” merely because people psychologically expect it.
Fun fact: guess what percent of Moderna study recipients who received a placebo (fake, totally harmless) vaccine reported side effects? 48%!
So a huge portion felt a side effect merely because they were expecting it.
Now, 48% is much less than the 88% of people who got the real Moderna vaccine and reported some side effect. But 48% from a pure nocebo effect is still massive.
We should expect something similar with “long Covid”. Perhaps, as with the vaccine, it’s half of the reported cases? Unfortunately we can’t answer that with any precision, because the few studies on this have very poor methodology.
Some have written on this, skipping over the methodological problems. For example, an op-ed in the NY Times says:
One peer-reviewed study of people who reported long Covid symptoms… The level of symptoms… was virtually the same whether the person was positive or negative for antibodies…
Another non-peer-reviewed study found that the rates of adolescents reporting symptoms such as fatigue and memory loss that are often attributed to long Covid were the same among those who had a mild SARS-CoV-2 infection and those who had not been infected, as ascertained by antibody testing.
By far the best of the studies mentioned there is that last one, on adolescents in Germany; it finds no difference in things like fatigue, concentration, and insomnia, when comparing teens who had Covid (antibodies) vs those who didn’t (no antibodies.) Unfortunately it didn’t consider the most common effect of smell/taste loss.
The study concludes clearly: “symptoms of Long-COVID19 might be less common than previously assumed.”
The German study is the best, because the antibody testing was actually done by the experimenter (not merely self-reported) and the scientists took seriously the meaning of an antibody test and even made an extra effort to pick up prior infection by doing multiple kinds of tests.
Unfortunately, the three studies of adults are far weaker — so weak that it’s hard to draw any conclusions; virtually everything (including the test results themselves) are based on self-reports via surveys, and furthermore the study authors fail to seriously differentiate between antibody and PCR tests. These problems broadly apply to the three studies.4
The excellent Scott Alexander — who has the best blog on the internet — suggests that studies refute claims similar to those above.
I feel like some of the case-control studies above, which clearly show that seropositive people have higher rates of Long COVID than seronegative people, are pretty convincing here.
However, going through the studies he lists, none of them look at people who thought they had Covid and then checked for antibodies — which would address the nocebo effect.
The Swedish healthcare worker participants were told whether they had antibodies or not — so this study would not have picked up a “nocebo effect” if it existed.
I confirmed with the Swedish researchers by email that the participants who were negative for antibodies were told they they tested negative — and that all hospital staff were recruited for the study, regardless of whether they thought they’d had Covid or not. The UK data has similar issues.
The nocebo effect probably exists, and we just don’t know how big of an effect it is.
Do vaccines help against “Long Covid”?
Yet another factor leaning against the danger of “long Covid” is vaccination. The above studies are based on pre-vaccination infections. Might vaccinated people fare better?
There isn’t great data yet on “long Covid” among vaccinated “breakthrough cases.” This small study of 39 such cases in Israel hints that “long Covid” isn’t so different among people who were vaccinated and then got Covid:
At 6 weeks after their diagnosis, 19% reported having “long Covid-19” symptoms, which included a prolonged loss of smell, persistent cough, fatigue, weakness, dyspnea, or myalgia
That’s a less than what the Swedish study found (26% had symptoms after 8 weeks, focusing on non-breakthrough cases.)
Better evidence comes from a much larger British study (2,370 breakthrough cases) which finds that the risk of symptoms 28 days out is halved for people who got both vaccine shots. This is only a partially-relevant finding, as 28 days is hardly true “long Covid”, but it’s quite plausible that’s closely correlated with real long Covid. We’ll have to wait a while to know for sure.
Overall, there’s good reason for optimism that all the risks described above are roughly halved for vaccinated people.
Conclusion: Covid impairment is LESS likely than most people think
The media headlines I’ve seen mislead people about the likelihood of Covid causing brain loss / impairment. Headlines about “long Covid” also mislead by failing to consider the nocebo effect seriously enough.
I’m glad I’d barely heard of “long Covid” back when I had Covid in September 2020. It would have sucked to be worrying extra about that, when the odds of any problem sticking around are so slim.
But everyone should judge for themselves how much they care about the small risk that “long Covid” poses.
I’ll add that one study found that the risk of “long” symptoms is 1.5x that of the flu. Goes to show that we’ve always been taking risks with our health; we’re just more conscious of these risks now, because of the novelty of Covid.
Avoiding Covid permanently is also looking increasingly difficult, as it becomes clearer and clearer that Covid is here to stay and is not going to be eradicated.
Regardless of your own conclusion, I hope this latest dig into the data helps you calibrate worries and make decisions.
Please subscribe to see future data deep dives! It’s free, and all my posts will always be free. But paid subscriptions also encourage me to do more of this in-depth research.
This is the second deep dive of many. Next up: multiple cities are considering getting rid of merit-based public schools. What’s the likely impact on learning, per the data?
DISCLAIMER: Above is not medical advice, but rather my best attempt to lay out the most important data using my statistics knowledge. If you see any NEW important data, or anything I missed, or any mistakes, please let me know in the comments.
Specifically, they show in figure 3 that just over 12% of people say they have “long Covid” and report any symptom (mostly fatigue and loss of smell) 4 months out. That’s quite close to the Swedish study after subtracting the control group’s reports (21.4% - 7.2% = 14.2%)
In all three studies, the studies find that people with “negative test results” have about as many symptoms as people who had positive test results — BUT because of atrocious methodology in how the define “negative test results” this tells us next to nothing; we still have no idea if these people who report long Covid symptoms actually had Covid or not.
Study 1: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8437054/
^ this paper has big problems.
First, it’s entirely based on self-identification of test results.
Second, doesn’t consider antibody tests at all. We have little idea who actually had Covid and who didn’t.
Third, it defines “long” as >4 weeks. That’s silly to have it that short — lingering cough, for example, often last more than that from regular colds. In my (pretty typical) case, sense of smell loss lasted 8 weeks. But I’d never have imagined thinking I had “long Covid” as a result.
This paper is not very useful for answering our question.
Study 2: https://www.medrxiv.org/content/10.1101/2020.11.04.20226126v1.full.pdf
^ this paper has big problems:
First, tiny sample size (89 people.)
Second, the population consists of relatively severe, hospitalized cases.
Third, and most critically, the paper fails to distinguish between antibody tests which can tell if someone has had Covid, and PCR tests, which must be done within a very narrow window to get a positive.
Fourth, even though it was in a hospital settings, everything was taken from patient self-reports.
The paper is not very useful for answering our question.
Study 3: https://www.thelancet.com/action/showPdf?pii=S2589-5370%2821%2900299-6
^ this paper has big problems.
First, survey was done among Facebook support groups for people with Long Covid; a particularly non-random population of people who are particularly focused on their ailment.
Second, it’s entirely based on self-identification of test results.
Third, the paper fails to distinguish between antibody tests which can tell if someone has had Covid, and PCR tests, which must be done within a very narrow window to get a positive. Actually they break this out in a descriptive stats table, but fail to break it out when it comes to actually important breakdowns in symptoms.
Not very useful.






I'm a 60 y/o, very healthy, slim man with no comorbidities and on no medications. I do take vitamin D, C, minerals, and a few other things which aren't relevant to covid. I had covid in July 2021 and felt headachy for a week, had a fever for 3 days, and lost nearly all my sense of smell. Here about 4 months later, my sense of smell and taste are mostly, but not 100% back. Yet I continue to notice progress. This weekend I noticed that my BF was wearing cologne, something I'd likely not have noticed a week or more ago. I've also started to notice smells walking around the city again. Initially very pessimistic about the loss of smell and taste (my cooking skills took a definite turn for the worse), I'm now optimistic that my smell will eventually return. Even nerves, notoriously hard to re-grow, will eventually come back.
Kim G
Roma Sur, Mexico City
It was possible to get much better results with much less sacrifice. Simply target restrictions, vaccines and treatments to the most vulnerable. This would get what was needed to those who needed it faster without watering that all down by forcing the much less vulnerable into the same line. The slow speed of response for the vulnerable due to trying to do everyone at once was the biggest killer Also allow experimentation with any treatment showing promise instead of limiting it to just the government approved ones. Simply do it with intelligence rather than panic, politics, and profits.